This supplementary report explores how regular COVID-19 booster campaigns might impact excess mortality in elderly populations across different ethnic groups in New Zealand.
By analyzing official population projections and observed post-vaccination mortality patterns, this work aims to inform policy decisions that balance public health goals with ethical
and demographic considerations.
Why Ethnicity Matters
New Zealand has a diverse population with varying health profiles. Māori communities, in particular, experience higher rates of chronic conditions and earlier onset of age-related disease.
It is vital that any policy involving medical interventions considers both absolute and relative risks across ethnic groups.
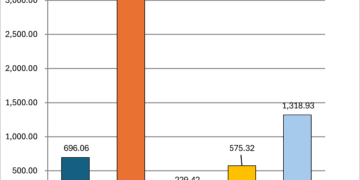
Data Sources and Methodology
We use Stats NZ’s medium-scenario population projections (2025–2035), broken down by age and ethnicity. Risk estimates are derived from post-vaccination mortality analyses in official
datasets from 2021–2024. The estimated per-dose excess mortality is:
– Age 65–79: 0.04%
– Age 80+: 0.15%
These are applied to booster scenarios of once per year, once every two years, and once every three years.
Māori Population (Ages 65–79)
Projected excess deaths rise over time, tracking cohort growth.
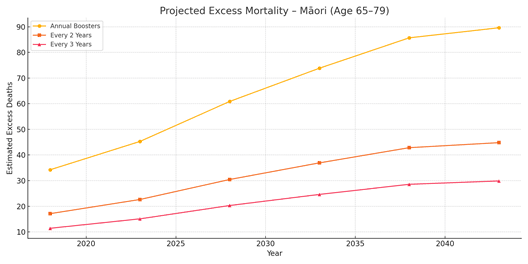
Figure 1: Māori 65–79 – Annual vs. Reduced Booster Frequency
Māori Population (Ages 80+)
Even with a smaller base, projections show meaningful impact due to high per-dose mortality and aging trends.
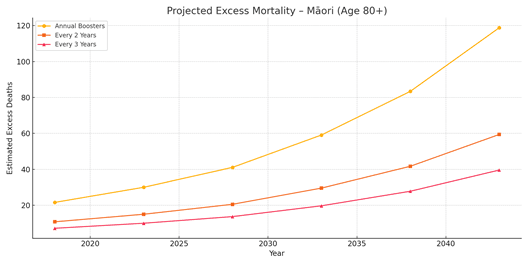
Figure 2: Māori 80+ – Annual vs. Reduced Booster Frequency
Other Ethnicities (Ages 65–79)
Larger population sizes yield more pronounced cumulative projections, even with moderate per-dose risks.
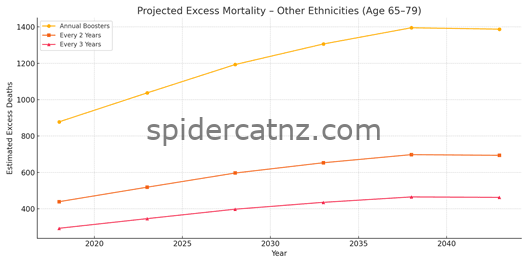
Figure 3: Other Ethnicities 65–79 – Annual vs. Reduced Booster Frequency
Other Ethnicities (Ages 80+)
This group constitutes the bulk of elderly NZers. The projected numbers indicate substantial future mortality under current policies.
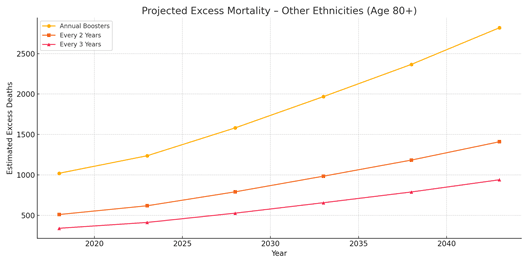
Figure 4: Other Ethnicities 80+ – Annual vs. Reduced Booster Frequency
Key Takeaways
– Reducing booster frequency significantly lowers projected mortality across all groups.
– Māori populations, while smaller, may experience disproportionate impacts due to health disparities.
– Future public health planning should consider differential risk profiles and focus on age- and health-specific protection strategies.
Next Steps
– Expand analysis to include real-world booster uptake data by ethnicity and health status.
– Consider integration with hospitalization and case severity data.
– Launch targeted outreach or exemption strategies where risk outweighs benefit.