A Rise in Uncertainty: Ill-Defined and Perinatal Infant Deaths in New Zealand
Overview
This article examines mortality classifications under ICD Chapter 18 (Ill-defined conditions) and Chapter 16 (Certain conditions originating in the perinatal period) for New Zealand children aged 0–4 between 2013 and 2022. The dataset shows that these deaths overwhelmingly occur in infants (age 0), with minimal contribution from ages 1–4.
Key Findings – Chapter 18: Ill-defined Causes
| Year | Age 0 | Age 00–04 | Age 1–4 (= 00–04 − 0) |
|---|---|---|---|
| 2013 | 24 | 25 | 1 |
| 2014 | 14 | 15 | 1 |
| 2015 | 19 | 23 | 4 |
| 2016 | 20 | 24 | 4 |
| 2017 | 29 | 31 | 2 |
| 2018 | 26 | 30 | 4 |
| 2019 | 39 | 45 | 6 |
| 2020 | 29 | 32 | 3 |
| 2021 | 39 | 40 | 1 |
| 2022 | 48 | 50 | 2 |
Infant deaths under Chapter 18 are entirely R95–R99 (unknown/unspecified causes) in every year (2013–2022).
The increase began by 2019 (39 deaths), dipped in 2020 (29), then rose again in 2021–2022 (39, 48).
Age 1–4 contributed only 1–6 deaths per year.
Thus, the “rise” in ill-defined causes was not a post-2020 phenomenon only; it was already evident by 2019 and is essentially confined to infants.
Key Findings – Chapter 16: Perinatal Conditions
| Year | Age 0 | Age 00–04 | Age 1–4 (= 00–04 − 0) |
|---|---|---|---|
| 2013 | 152 | 152 | 0 |
| 2014 | 175 | 176 | 1 |
| 2015 | 123 | 123 | 0 |
| 2016 | 134 | 134 | 0 |
| 2017 | 151 | 151 | 0 |
| 2018 | 141 | 142 | 1 |
| 2019 | 135 | 136 | 1 |
| 2020 | 151 | 152 | 1 |
| 2021 | 180 | 181 | 1 |
| 2022 | 162 | 164 | 2 |
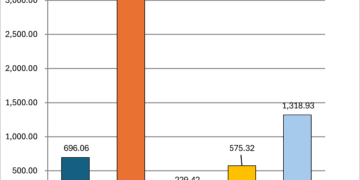
Selected Age-0 subgroup series (deaths per year):
| Year | P05–P08 (Gestation/ Growth) | P20–P29 (Resp/Cardio) | P90–P96 (Other perinatal) | P50–P61 (Haem/Haemato) | P35–P39 (Infections) |
|---|---|---|---|---|---|
| 2013 | 64 | 39 | 14 | 15 | 12 |
| 2014 | 91 | 31 | 17 | 17 | 12 |
| 2015 | 44 | 31 | 21 | 10 | 12 |
| 2016 | 56 | 24 | 24 | 9 | 10 |
| 2017 | 71 | 32 | 18 | 15 | 8 |
| 2018 | 68 | 21 | 15 | 12 | 13 |
| 2019 | 67 | 25 | 21 | 10 | 5 |
| 2020 | 68 | 19 | 24 | 20 | 15 |
| 2021 | 75 | 18 | 41 | 13 | 23 |
| 2022 | 51 | 25 | 44 | 16 | 19 |
P05–P08 (Gestation/fetal growth issues): Large spike in 2014 (91 deaths). The Ministry of Health has stated this was a “catch-up” year, reflecting previously unentered deaths being added into the registry. A second rise occurs in 2021 (75), but unlike 2014 it is not accompanied by an official note of data correction. In 2022, P05–P08 drops to 51.
P90–P96: Clear rise post-2020 (24 → 41 → 44).
P35–P39: Rise post-2020 (15 → 23 → 19).
P20–P29: Stable to declining until 2021, small increase in 2022 (25).
P50–P61: Fluctuating, not steadily increasing (peaked in 2020 at 20).
Again, virtually all perinatal deaths are in infants; Age 1–4 contributes at most 1–2 per year.
Population Context
Stats NZ age-0 population estimates show the 2021 cohort was modestly larger (61,060) than surrounding years (typically ~59,000–60,000). This does not explain the post-2020 rises in Chapter 16 subgroups such as P90–P96 and P35–P39.
Corrected Interpretation
Chapter 18: Infant ill-defined deaths (R95–R99) were already rising by 2019, not only after 2020.
Chapter 16: Certain perinatal subgroups (P90–P96, P35–P39) show real rises after 2020, but P05–P08’s 2014 spike is a documented catch-up artifact rather than a sudden mortality surge. Its 2021 increase does not carry the same administrative explanation.
These shifts remain almost entirely confined to infants (age 0).
Data Source: Ministry of Health NZ, mortality_Chapt_Subgrp.txt (2013–2022).
Were More Babies Born?
To test whether these increases might simply reflect a growing infant population, we examined annual average birth cohort sizes (proxied by age 0 population):
| Year | Average Age 0 Population |
| 2013 | 59,858 |
| 2014 | 58,370 ⬇️ |
| 2015 | 59,018 |
| 2016 | 59,718 |
| 2017 | 59,958 |
| 2018 | 59,408 |
| 2019 | 59,808 |
| 2020 | 59,238 |
| 2021 | 61,060 ⬆️ |
| 2022 | 59,855 |
The 2021 birth cohort was modestly larger than surrounding years, but not enough to explain the sharp post-2020 increases in infant deaths. 2020 and 2022 were typical and align with pre-pandemic norms.