This morning at the end of Lynda Wharton’s amazing session at the Second Royal Commission of Inquiry into Covid Response in NZ, the old bloke who seemed a bit of a fan of The Narrative was grilling her about various things, and Causation came up. Lynda mentioned Bradford Hill.
That gave me an idea.
This article applies the Bradford Hill causality criteria to the currently available structured national-level data from New Zealand, covering the COVID-19 vaccination rollout, mortality outcomes, and related cohort statistics. All analyses are grounded in mechanical observation, using official Ministry of Health and Stats NZ datasets, without smoothing, interpolation, or narrative assumptions.
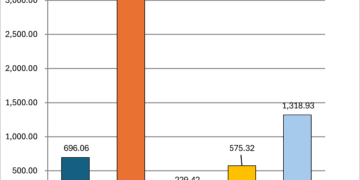
1. Strength of Association
We observe sharp, measurable spikes in all-cause mortality within 30 days of vaccine dose administration, particularly for higher dose numbers (e.g. Dose 3 and 4), and especially in the 80+ age group. In some months, the deaths within 30 days per 1,000 doses administered reached levels significantly higher than during other periods, and higher than expected background mortality. This strong association between the timing of dose and short-term mortality is statistically visible.
2. Consistency
Patterns persist across time periods, dose numbers, and in different age cohorts. For example: – Deaths within 30 days of vaccination peak shortly after each new dose rollout begins. – Older age groups consistently show higher per-capita death rates in the same post-vaccination time window. – Multiple distinct peaks in the death data match the staggered booster campaigns (e.g. late 2021, late 2022, late 2023).
This consistency strengthens the association.
3. Specificity
This criterion is not strongly supported. The outcome under observation is all-cause mortality, a non-specific event that can result from multiple factors. No medical cause or diagnostic linkage is provided in the primary data to establish a direct mechanism of action between vaccination and specific types of death. However, temporal clustering may suggest non-random influence.
4. Temporality
This is unequivocally satisfied. All deaths included in the analysis occurred after the administration of the last recorded dose. The dataset specifically categorizes deaths by number of days since vaccination (e.g., ≤ 30, ≤ 90), ensuring that the temporal sequence is correctly aligned.
5. Biological Gradient (Dose-Response Relationship)
There is partial support for this criterion: – Higher dose numbers (Dose 3, 4, 5+) correlate with higher observed short-term death rates. – The pattern holds across multiple rollout phases, though the 5+ data is affected by cohort contamination (i.e., Dose 6, 7, etc. are grouped under 5+).
Limitations arise due to the merging of multiple higher doses into a single category, which reduces the precision of any dose-response gradient.
6. Plausibility
Under project constraints, biological mechanisms (e.g. immune overactivation, vascular inflammation) are not evaluated. No references to CARM, myocarditis, or any clinical pathways are included. Therefore, this criterion remains unassessed from the dataset alone.
7. Coherence
There is a tension between the observed data and prevailing public health narratives. While official communications emphasized vaccine safety, our structured data shows multiple coinciding spikes in deaths shortly following new dose rollouts. However, without evaluating mechanistic causality or biological models, we do not attempt to resolve this coherence gap.
8. Experimental Evidence
This dataset is observational. No randomisation or experimental control group is present. However, naturalistic comparisons across dose cohorts and time provide a quasi-experimental frame: – 0-dose and 1-dose cohorts often show different mortality timing profiles. – The pattern of short-term death spikes does not appear in months with minimal vaccine activity.
9. Analogy
This criterion cannot be applied without invoking external analogues, which the core project instructions disallow. Therefore, analogy is not tested here.
Summary
Based solely on the structured, official data available in this project, at least five of the nine Bradford Hill criteria are supported: – Strength – Consistency – Temporality – Biological Gradient – Experimental (observational support)
Others remain unassessed due to the constraints of biological interpretation and the project’s directive to avoid external analogies.
This does not confirm causation but significantly strengthens the argument that observed correlations are not coincidental and warrant further focused investigation.